Article by Tommy Leong, President, Schneider Electric East Asia & Japan.
We are living longer, and better, in Asia than we have ever done before, but this is resulting in soaring demand for healthcare providers in the region to deliver high-quality medical care, consistently and sustainably. The World Bank reports that East Asia’s population is ageing faster than any other region in history, with 36 percent of the world’s population (211 million people) over the age of 65—namely, Singapore, Japan, and South Korea are considered as “advanced agers”, while other fast-ageing countries include China, Indonesia, Thailand, and Vietnam.[1] Further, the increasing prevalence of chronic diseases add to the demands on healthcare organisations, which are already constrained by tightening budgets and a lack of resources.
To meet the demands of an ageing population, there is an even greater focus to achieve better operational efficiency, while improving patient safety and satisfaction through integrating innovative technology inhealthcare infrastructure. The World Health Organisation’s (WHO) “Global Strategy on Human Resources for Health: workforce 2030” agenda reinforces technological innovation as a mean to improve and strengthen national health systems in today’s “Big Data” era[2]. Meanwhile, hospitals on average use three times the volume of electricity than that of a typical large-scaled office building, thereby adding to the burden of rising operating and energy costs.
Whether designing a new facility or expanding an existing one, hospitals and healthcare amenities are under mounting pressure to do more with less. In addition, it is important to consider prudent investment in technological healthcare solutions that deliver quality care, patient safety, hospital security, and staff productivity.
Creating a Future-ready Hospital
An optimally designed hospital needs to accommodate the use of sophisticated equipment; allow for rapid responses to emergencies; include built-in protection against human errors and mechanical failures; as well as provide safe spaces for patients to heal and the clinical staff to work.The answer to this is a Digital Healthcare Infrastructure, called EcoStruxure™ for Healthcare, which uses the latest technology including: 1) Embedded connectivity and intelligence; 2) Smart control, management, automation and optimisation; and 3) Cloud-based digital services. Acting as the central nervous system of a hospital, the EcoStruxure for Healthcare bridges the Information Technology (IT)/Operational Technology (OT) gap and connects the three core layers of connected products, monitoring and control software, as well as apps and analytics—therefore building efficiency across an organisation to create a ‘future-ready’ hospital.
The intelligent infrastructure integrates and enables communication between traditionally disparate systems, leading to greater utilisation and ROI (Return On Investment) of “connected” infrastructure devices – or IoT (Internet of Things) such as temperature sensors, power meters, building automation controllers, real-time location system devices, and more. These IoT-enabled devices provide several benefits including embedded intelligence and control, control and monitoring capabilities via the cloud, as well as advanced analytics with the help of software. Data collected from connected devices is used to drive better decision making and process improvements.
For instance, a clinical environment optimisation solution can share the occupancy status of patient rooms and operating theatres with the Building Management System (BMS), which then sets rooms to predetermined set points for HVAC and lighting during vacancy to achieve energy savings during unoccupied times. The BMS puts the room back into normal operation when it receives a notification that the patient will be returning or when a room has been assigned to maintain the optimal environment for patient healing and satisfaction.
In Singapore, a notable example of how intelligent technology infrastructure is enabling health services to grow and meet patient demand, can be seen in Integrated Healthcare Innovation Systems’ (IHIS) adoption of Schneider Electric’s Data Center Infrastructure Management (DCIM) solution. The solution was part of IHIS’ private health cloud, H-Cloud, developed to replace legacy IT silos and provide a disaster resilient platform for electronic medical records across six of Singapore’s regional health systems. An independent assessment by PwC suggests that the health cloud will deliver millions of dollars’ worth of savings over the next ten years. Each hospital cluster will reduce its costs by nearly 55 percent, compared to business-as-usual costs, by 2025.
Improve Senior Patient Care and Experience
At hospitals, the stakes are high: 1) Uninterrupted access to power or a power outage can mean the difference between life and death, and with an average cost of greater than $1 million for a 200-bed hospital; and 2) Adverse patient events (APEs) and healthcare-associated infections (HAIs) continue to claim lives, with attributed mortality in infected patients in hospitals in Southeast Asian countries at an estimated range of 7 percent to 46 percent[3].
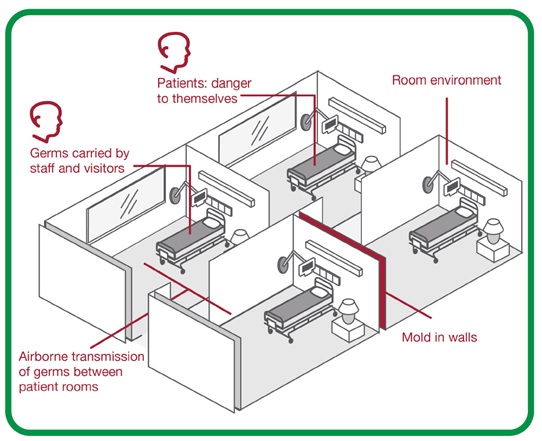
The good news is, proper safeguards can reduce these APEs and HAIs, medical errors, and patient falls.
Automated testing of electrical distribution system and emergency power supply systems (EPSS) counteract the consequences of human error. By improving the electrical distribution system reliability, hospitals can both improve patient safety and reduce the financial risk of malpractice and wrongful death suits. Automated systems also ensure compliance to regulations and produce compliance reports.
To minimise the need for extra maintenance personnel and adding to operational expenses, hospitals can build intelligence into their ventilation systems to optimise patient safety and maintenance. The intelligent system will automatically monitor and maintain humidity, ventilation, air pressure, and HEPA filters in real-time, and ensure they are controlled to design requirements.
For healthcare providers, there is value in delivering a high-quality, positive and engaging patient experience. For example, a hospital with $120 million annual revenue can improve patient satisfaction and realise an estimated $2.2 million to $5.4 million in additional revenue annually.[4]
Digital innovation transforming elderly healthcare
Patient safety starts at the very foundation – the physical foundation – of hospital facility systems. As people are getting older and experiencing multiple chronic diseases, they require a new paradigm of treatment in hospitals and clinics as well as at home.
On the operational front, healthcare facilities must find a way to work better and smarter, and do more with less. Energy efficiency projects can unlock trapped capital that can improve a hospital’s profit margin or be used to fund technological advancements, purchase medical equipment, or improve the patient experience—vital elements that would deliver significant results in terms of cost savings and patient-centric improvements. With 54 percent of healthcare executives ranking patient experience and satisfaction among their top three priorities[5], as well as the availability of automated solutions to enable an intelligent healthcare infrastructure, future-ready hospitals may very soon become a widespread reality than an experimental concept.
By embracing intelligent infrastructure and applications, East Asian nations will have a solid foundation to transform the future of health and social care for its golden-agers. Schneider Electric believes that intelligent technology is the answer, and it is a solution that healthcare organisations can successfully achieve today.
[1]World Bank. 2016. Live Long and Prosper: Aging in East Asia and Pacific. Washington, DC: World Bank.
[2]World Health Organisation. 2016.Global strategy on human resources for health: workforce 2030. Geneva, Switzerland: WHO.
[3]Ling ML, Apisarnthanarak, A, Madriaga, G. (2015). “The Burden of Healthcare-Associated Infections in Southeast Asia: A Systematic Literature Review and Meta-analysis,” Clinical Infectious Diseases, 60(11), 1690-9.
[4]Hall, MF. (2008). “Looking to Improve Financial Results? Start by Listening to Patients,” Healthcare Financial Management,62(10), 76-80.
[5] “2013 Industry Survey Data,” HealthLeadersMedia, (2013).








